Good health should be a fundamental right, not a privilege determined by your background or circumstances. The pursuit of health equalities is a cornerstone of a fair and just society, aiming to ensure that everyone has the same opportunity to lead a healthy life. This concept moves beyond simply providing equal access to healthcare; it addresses the underlying social, economic, and environmental factors that shape our well-being from birth. Understanding the landscape of health equalities is the first step toward building healthier, more resilient communities for everyone.
This guide will break down what health equalities mean, distinguish the concept from health equity, and explore the deep-rooted factors that create unfair health outcomes. We will look at real-world examples and outline the practical steps that individuals, communities, and governments can take to close the health gap and create a system where fairness is the standard.
Defining Health Equalities vs. Health Equity
The terms “health equality” and “health equity” are often used interchangeably, but they represent distinct and important concepts. Grasping the difference is crucial for effective policymaking and community action.
What are Health Equalities?
Health equalities refer to the goal of ensuring everyone has the same opportunities to attain their full health potential. It implies that no one should be disadvantaged from achieving this potential because of their social position or other socially determined circumstances. Essentially, it’s about leveling the playing field so that factors like race, income, or location do not predetermine a person’s health outcomes. The focus is on the outcomes being the same for all groups.
What is Health Equity?
Health equity is the process through which health equalities are achieved. It involves providing everyone with what they need to be healthy, which means distributing resources fairly, but not necessarily equally. Equity recognizes that some groups have been systematically disadvantaged and require more support or different resources to reach the same starting line as others.
- Equality: Giving everyone the same pair of shoes.
- Equity: Giving everyone a pair of shoes that fits them perfectly.
In practice, we strive for health equity to achieve a state of health equalities. For the remainder of this guide, while we focus on the goal of health equalities, we will often discuss the equitable actions needed to get there.
Why Do Health Inequalities Persist? The Social Determinants of Health
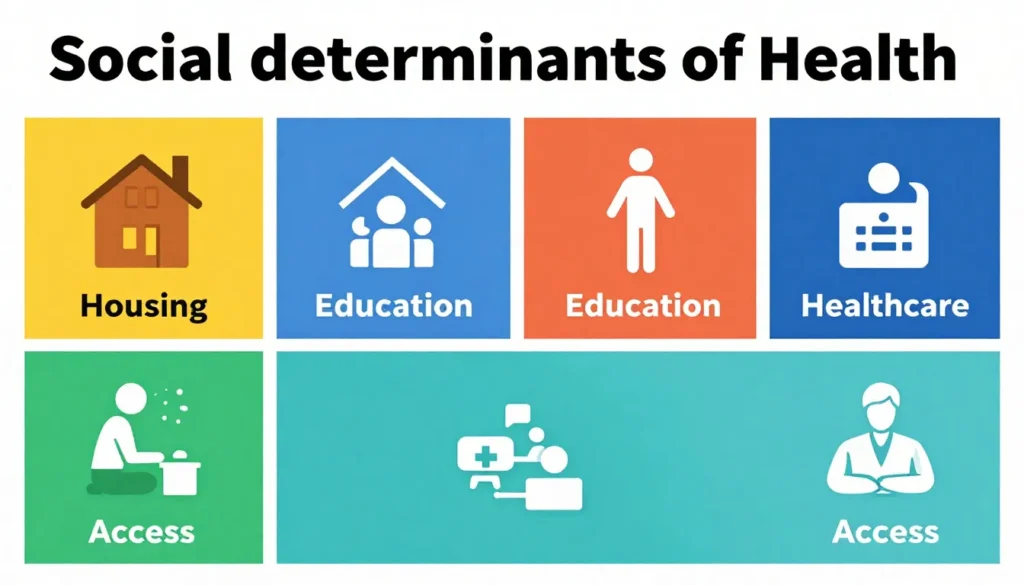
Health is not made in a doctor’s office; it is made in our homes, schools, and communities. The conditions in which we are born, grow, live, work, and age are known as the social determinants of health. These factors are the primary drivers of health inequalities.
1. Economic Stability
Poverty is one of the most significant barriers to good health.
- Income and Employment: A stable income allows for access to healthy food, safe housing, and healthcare services. Job insecurity and low wages create chronic stress, which has profound physiological effects.
- Food Insecurity: Lack of access to affordable, nutritious food often leads to diets high in processed foods, increasing the risk of obesity, diabetes, and heart disease.
- Housing Instability: Unsafe or unstable housing conditions, such as exposure to lead, mold, or overcrowding, directly impact health. Homelessness represents an extreme health risk.
2. Education Access and Quality
Education provides the knowledge and skills needed for a stable career, which in turn influences economic stability and health literacy.
- Early Childhood Development: Quality early education sets the foundation for lifelong learning and better health outcomes.
- Health Literacy: The ability to understand and use health information is critical for managing personal health. Lower educational attainment is often linked to lower health literacy, making it difficult to navigate the healthcare system.
3. Healthcare Access and Quality
While not the only factor, access to quality healthcare is a critical determinant.
- Lack of Insurance: Individuals without health insurance are less likely to receive preventative care and may delay seeking treatment until a condition becomes a crisis.
- Geographic Barriers: People in rural areas often have to travel long distances to see a doctor or specialist, creating a significant barrier to care.
- Cultural Competence: A lack of cultural competence among healthcare providers can lead to mistrust, poor communication, and misdiagnosis, particularly affecting minority ethnic groups.
4. Neighborhood and Built Environment
The physical environment of a community has a profound impact on its residents’ health.
- Access to Healthy Foods: “Food deserts”—areas without access to full-service grocery stores—are common in low-income neighborhoods.
- Safety: High crime rates can lead to chronic stress and limit outdoor physical activity.
- Environmental Conditions: Exposure to pollution from factories or highways is often higher in marginalized communities, leading to increased rates of asthma and other respiratory illnesses.
5. Social and Community Context
Our social connections and the community we live in provide support systems that are vital for both mental and physical health.
- Social Cohesion: A sense of community and belonging can buffer against the negative effects of stress.
- Discrimination and Stigma: Systemic racism and other forms of discrimination create chronic stress and act as significant barriers to accessing education, employment, and healthcare.
- Civic Participation: Communities where residents have a voice in local decisions are more likely to have policies that promote health.
Real-World Examples of Health Inequalities

Examining specific examples helps illustrate how the social determinants of health create tangible disparities.
The Life Expectancy Gap
In many cities around the world, there can be a 10-20 year difference in life expectancy between residents of wealthy neighborhoods and those in low-income areas just a few miles away. This stark gap is not due to genetics but to decades of disparity in access to resources and opportunities.
Maternal Mortality Rates
In the United States, Black women are three to four times more likely to die from pregnancy-related causes than white women, regardless of income or education level. This points to the impact of systemic racism, implicit bias within the healthcare system, and the cumulative stress of discrimination on maternal health.
Diabetes and Socioeconomic Status
Type 2 diabetes is significantly more prevalent among low-income populations. This is linked to a combination of factors, including limited access to healthy foods, fewer opportunities for safe physical activity, and higher levels of chronic stress associated with financial instability.
COVID-19 and Health Disparities
The COVID-19 pandemic laid bare the deep-seated health inequalities in our societies. Low-income and minority communities experienced disproportionately higher rates of infection, hospitalization, and death. This was driven by factors such as:
- Living in crowded, multigenerational housing.
- Working in frontline jobs with high exposure risk.
- Higher rates of underlying health conditions like hypertension and diabetes.
- Limited access to testing and quality care.
Strategies for Promoting Health Equalities
Tackling health inequalities requires a multi-faceted approach that addresses the root causes. It involves action from governments, healthcare systems, community organizations, and individuals.
1. Strengthening Policies that Address Social Determinants
True progress toward health equalities starts with policy change.
- Economic Policies: Implementing living wage laws, expanding earned income tax credits, and strengthening unemployment benefits can improve economic stability for families.
- Housing Policies: Investing in affordable housing, enforcing safe housing codes, and preventing evictions are crucial for public health.
- Education Funding: Equitably funding public schools ensures all children have access to quality education, regardless of their zip code.
2. Transforming the Healthcare System
The healthcare system must move from a treatment-focused model to one centered on prevention and equity.
- Universal Health Coverage: Ensuring everyone has access to affordable health insurance is a foundational step.
- Promoting Cultural Competence: Healthcare organizations must invest in training for providers to recognize and address their own biases, improving patient-provider communication and trust.
- Integrating Social Care: Clinics and hospitals can screen patients for social needs (like food or housing insecurity) and connect them with community resources.
3. Community-Led Initiatives
Local communities are often best equipped to identify and solve their own health challenges.
- Community Health Workers: These are trusted community members who act as a bridge between residents and the healthcare system, helping people navigate services and manage their health.
- Building Healthy Environments: Community gardens, farmers’ markets in food deserts, and advocacy for safe parks and bike lanes can transform local environments.
- Empowering Local Voices: Supporting community-led organizations and ensuring residents have a seat at the table in local governance are key to creating sustainable change.
4. Leveraging Data and Technology
Data is essential for identifying where inequalities exist and measuring the impact of interventions.
- Disaggregated Data: Collecting health data broken down by race, ethnicity, income, and geography helps pinpoint specific disparities.
- Telehealth Expansion: While not a solution for everyone, telehealth can improve access to care for people in rural areas or those with mobility issues, provided the digital divide is addressed.
Conclusion:
The pursuit of health equalities is not merely a task for public health departments or hospitals; it is a collective responsibility that touches every aspect of society. The existence of health inequalities is a sign of systemic failures that limit human potential and create a less stable, less prosperous world for everyone.
By focusing on health equity—providing tailored support to address historical disadvantages—we can begin to dismantle the barriers that prevent so many from living long, healthy lives. This means investing in education, advocating for fair economic policies, redesigning our communities for well-being, and demanding a healthcare system that treats everyone with dignity. The path to a healthier future is one where fairness and opportunity are not just ideals, but realities for all.
FAQs
What is the difference between health inequalities and health inequities?
Health inequalities are the observable differences in health outcomes between different groups of people (e.g., life expectancy). Health inequities are those inequalities that are avoidable, unfair, and unjust, arising from systemic issues like discrimination or unequal distribution of resources.
Are health equalities just about access to doctors?
No. While access to healthcare is important, it is only one piece of the puzzle. The social determinants of health—such as income, education, housing, and environment—are much larger drivers of health outcomes. Achieving health equalities requires addressing these root causes.
How can one person help promote health equalities?
Individuals can make a difference by:
- Educating themselves on the social determinants of health.
- Advocating for policies that support health equity (e.g., affordable housing, living wages).
- Volunteering with or donating to community organizations working on these issues.
- Challenging stigma and discrimination in their own communities and workplaces.
Is achieving perfect health equality possible?
While eliminating all differences in health may not be entirely possible (due to factors like genetics), achieving health equalities by removing unfair, systemic barriers is a tangible and necessary goal. The aim is to ensure that everyone has the opportunity to be as healthy as possible.
Why does health equality matter for the economy?
Health inequalities are costly. A sicker population is less productive, and managing chronic diseases driven by social factors places a huge financial burden on the healthcare system and taxpayers. Investing in health equity is an investment in a stronger, more resilient economy.
Sofia Bennett is a fashion writer and style observer known for her clean sense of aesthetics and trend analysis. She has covered fashion shows, reviewed designer collections, and interviewed independent creators. Sofia specializes in connecting fashion with real-life lifestyle choices, helping readers understand what looks good — and why.